Making access to cancer clinical trials more affordable
The University of Texas Southwestern Medical Center
David Gerber, M.D.
Dallas, Texas

Dr. David Gerber, UTSW (Courtesy of UTSW)
As clinical trials become more complex, with increasing numbers of required procedures and clinic visits, gaining access to promising new treatments is even more challenging for many individuals. Financial barriers, like travel costs for participants, limit who is able to participate in a cancer clinical trial. Individuals with annual household incomes below $50,000 are 30% less likely to enroll in cancer clinical trials than those earning more, and fewer than five percent of trial enrollees are Medicaid recipients. This is a critical problem because obstacles to participation may affect the time it takes to complete the cancer clinical trial and the diversity of the enrolled patient pool, both factors which ultimately impact the likelihood of regulatory approval for the new drug.
Through two key awards, CPRIT has created a comprehensive approach to increase access to clinical trials, ensuring that innovative treatments reach patients throughout Texas.
Following passage of HB3147 by the 86th Texas Legislature, CPRIT approved a first-of-its kind $1.5 million CPRIT Texas Clinical Trials Participation Program Award (RP210115) to The University of Texas Southwestern Medical Center in 2021 to fund an outreach program to increase clinical trial enrollment and reimburse nonclinical costs (e.g., travel, parking fees, lodging) for income-eligible patients participating in clinical trials. The UT Southwestern project, under the direction of David Gerber, M.D., is available to eligible patients participating in cancer clinical trials at UT Southwestern, Parkland Health, and Children’s Health. Although the COVID-19 pandemic affected the early roll-out of the project, to date it has provided over $170,000 in reimbursements to hundreds of patients participating in cancer clinical trials.
CPRIT awarded a $3 million CPRIT Clinical Trials Network Award (RP220542) in 2022 to UT Southwestern for the project “Accelerating Clinical Oncology Research Network - Texas (ACORN-TX).” ACORN-TX improves clinical trial access by partnering with network affiliate sites Baylor Scott & White Health in Temple and John Peter Smith Hospital in Fort Worth. These network affiliates are committed to clinical research and serve populations lacking cancer clinical trial options, including those in rural parts of the state and vulnerable populations who are low-income, underinsured, uninsured, and/or racial/ethnic minority groups.
By expanding the geographical reach of cancer clinical trials and building capacity at smaller institutions in north and central Texas, ACORN-TX increases access to innovative clinical trials and enhances the conduct and oversight of clinical trials.
LEARN MORE:
Enhancing access to and diversity in cancer clinical trials through a financial reimbursement and outreach program
Establish the Accelerating Clinical Oncology Research Network - Texas (ACORN-TX) to enhance clinical trial access in North and Central Texas
Creating a Cancer Prevention Ecosystem Across 104 Texas Counties
Moncrief Cancer Institute
Keith Argenbright, M.D.
Fort Worth, Texas
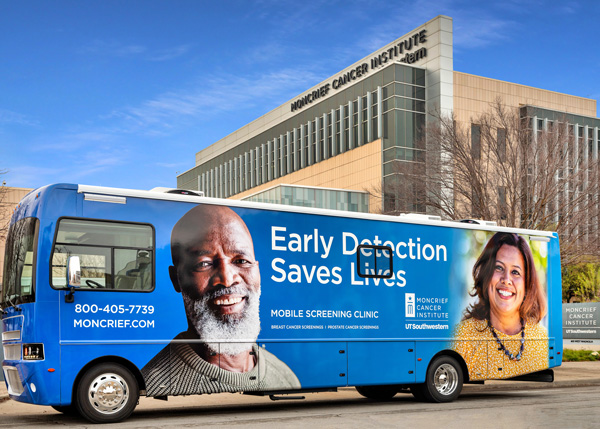
Mobile Screening Clinic (Courtesy of Moncrief)
“Because of CPRIT funding, we have screened thousands of men and women for cancer and have saved many lives through early detection. We are grateful for the partnership with CPRIT and for the privilege of providing cancer screening services for our fellow Texans.”
Dr. Keith Argenbright
Director of Moncrief Cancer Institute
Since 2010, 16 CPRIT-funded prevention programs run by the Moncrief Cancer Institute at The University of Texas Southwestern Medical Center under the direction of Keith Argenbright, M.D., have detected nearly 2,600 cancers and cancer precursors. The successful collaboration has assembled a formidable cancer prevention infrastructure across 104 North, Central and East Texas counties that is saving lives and shaping futures.
The Moncrief Cancer Institute and Dr. Argenbright received one of the first CPRIT prevention grants in 2010, beginning a longstanding partnership between CPRIT and Moncrief to provide education, cancer screenings, diagnostics, and navigation services in medically underserved areas. To effectively reach Texans across a service area equivalent in size to the state of Minnesota, Moncrief’s community outreach team engages leadership and screening providers in each county, identifies communication channels to reach priority populations, and collaborates with local interest groups.
Moncrief’s 16 prevention programs, totaling more than $32 million in CPRIT funding, include screening services for breast, cervical, colorectal, and lung cancer.
The breast cancer screening and navigation program, now on its sixth CPRIT grant (PP230013), serves women in 67 North and Central Texas counties. Using two Mobile Screening Clinics and a network of rural providers, Moncrief brings vital breast and cervical cancer screenings to areas without these services. Since the first grant in 2010, the program has provided over 85,000 clinical services and detected more than 1,250 cancers.
- The cervical cancer screening program provided services for women in 35 counties with the 2017 prevention grant (PP170010), which Moncrief expanded to 67 counties in 2020 (PP200064). The program has detected 450 cancer precursors and 15 cancers in the past seven years.
- The colorectal cancer screening and navigation program (PP240019 and PP220034) serves men and women in 87 counties in North, Central, and East Texas. Since the program began in 2010, Moncrief has provided more than 40,000 colorectal screenings, detecting more than 800 cancer precursors and 65 cancers.
- CPRIT first funded the lung cancer screening program in 2018 (PP180025), initially serving 18 counties. Moncrief expanded the program to serve 62 counties in North, Central, and East Texas through two additional grants (PP210042 and PP250019). To date, the program has provided more than 4,500 screenings and detected 54 cancers, helping to improve early detection and outcomes for men and women across the region.
LEARN MORE:
Cervical Cancer Screening and Patient Navigation (X-SPAN)
Lung Cancer Screening and Patient Navigation (LSPAN)
Disseminating Cancer Control Framework and Strategies, a UT System Partnership
The Expanded C-SPAN Coalition: Colorectal Screening and Patient Navigation
A Regional Expansion of Cervical Cancer Screening and Patient Navigation in North Texas (E-XSPAN)
A Regional Expansion of Lung Cancer Screening and Patient Navigation (E-LSPAN)
Community Expansion and Re-engagement for Breast Cancer Screening and Patient Navigation
Increasing Access to Successful Colorectal Cancer Screening, Pairing Patient Education and Outreach with Navigation
Saved by the Scan: Lung Cancer Screening and Patient Navigation in East Texas
Hypothesis to Market: The Development of the MasSpecPen
The University of Texas and MS Pen Technologies
Livia Schiavinato Eberlin, Ph.D.
Austin, Texas

Dr. Livia S. Eberlin in the lab
(Courtesy of Baylor College of Medicine)
For more than a century, doctors have used biopsies – minimally invasive surgical procedures that remove small pieces of suspicious tissue - to test for cancer cells and diagnose cancer. Analyzing these small samples can be challenging, expensive, and time-consuming, particularly if the surgeon fails to remove enough tissue for clear margins during the initial procedure. For the patient, waiting a week or more for the biopsy results can feel like a lifetime.
In 2016, The University of Texas at Austin and Livia Schiavinato Eberlin, Ph.D., assistant professor in the Department of Chemistry, received a $200,000 CPRIT High Impact/High Risk grant (RP160766) to develop an innovative chemical technique to directly analyze biopsies, and provide real-time diagnostic molecular information about lung cancers.
That technology led to the development of the MasSpec Pen, a break-through device for real-time tissue sensing and surgical guidance using mass spectrometry. The MasSpec Pen employs a “touch-and-know” approach to analyze suspicious tissue. During the biopsy, the surgeon uses a small pen-like tool to release a drop of water onto the suspicious tissue, causing small molecules to migrate into the water. The device sends the water sample into a mass spectrometer, which detects the sample’s unique molecular composition and creates a molecular fingerprint. The MasSpec Pen quickly distinguishes between benign and malignant cells, delivering results in about 10 seconds—more than 150 times faster than existing technology.
CPRIT awarded UT Austin and Dr. Eberlin a $983,000 Early Translational Research grant (RP170427) in 2017 to evaluate the efficacy of mass spectrometry tissue analysis for detecting thyroid cancer, a fast-rising cancer and one of the most difficult to biopsy. Dr. Eberlin, now at Baylor College of Medicine, continued to develop the technology with a $241,000 CPRIT Individual Investigator Clinical Translation grant (RP180381) to analyze ovarian cancer tissues and identify metabolic signatures to predict how a patient responds to surgery or to a specific treatment option.
When Dr. Eberlin was ready to take the MasSpec Pen to market, she again turned to CPRIT. In 2024, CPRIT awarded a $2.7 million Product Development Research grant to MS Pen Technologies, Inc., to commercialize the MasSpec Pen for cancer detection.
The MasSpec Pen is so revolutionary that it even captured the imagination of Hollywood producers, who featured the device in an episode of the television show, Grey’s Anatomy in 2018. Developers are exploring other uses of the MasSpecPen outside of medicine, including food authentication, agriculture, forensics, manufacturing quality control.
The story of the development of the MasSpec Pen highlights the vital role of CPRIT in driving innovation across the spectrum of cancer research, from hypothesis to market commercialization.
LEARN MORE:
Ambient Mass Spectrometry for Preoperative Molecular Diagnosis of Thyroid Fine Needle Aspirate Biopsies
Mass Spectrometry Imaging to Uncover Predictive Metabolic Markers of Ovarian Cancer Surgical Outcome and Treatment Response
Development of the Ultimate Surgical Sensing System for Intraoperative Tissue Sensing and Surgical Guidance